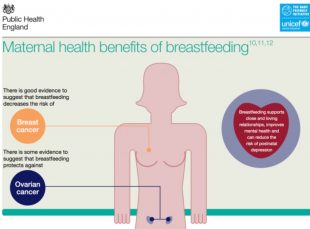
 This week we are celebrating breastfeeding, this gives a real opportunity to focus on the benefits and impact on long term outcomes for both mother and baby including healthy weight, protection from infection and safety.
This week we are celebrating breastfeeding, this gives a real opportunity to focus on the benefits and impact on long term outcomes for both mother and baby including healthy weight, protection from infection and safety.
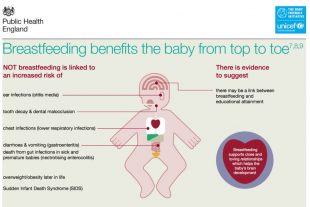
World Health Organisation recommends that babies are exclusively breastfed for the first six months and after that given a combination of breast milk and other food. But statistics for 2016/17 show that in England, only 44.4% of babies are still being breastfed when they are approaching 2 months old.
Nationally and internationally, breastfeeding is recognised as important and recommended that babies are exclusively breast fed for the first 6 months.
We hope the week provides an opportunity for mothers, breastfeeding supporters and health professionals to come together and share what works well to support breastfeeding in local communities in order to create a more breastfeeding friendly culture. It is a fantastic opportunity to show case all the good work that is happening across the country, share ideas, inspire others and promote the support available to women and their families.
Over the week we will be posting a number of blogs including those from key partners emphasising the importance of breast feeding and also sharing the support available for mums. We want health professionals and other key partners to share their local practice examples to encourage others to think about their role in breastfeeding.
Understanding the mother’s choice and what influenced her decision to breastfeed or not is really important, so we will share feedback from mums, to gain deeper insight and understanding of how we can support mothers better. We need to think together about creating and promoting a breastfeeding friendly community, so women are able to breastfeed or express milk without worry in the workplace, go out and about with their babies knowing they will easily find a convenient place where they can both have lunch, and share great ideas for community resources that support mothers and babies in their breastfeeding relationship.
Health care professionals including midwives, health visitors and general practices nurses can offer immense support; there is also other support available for example, peer support and helplines including the National Breastfeeding Helpline . Mothers may also opt for digital approaches including on-line support and digital solutions like the Start4Life Breastfeeding Friend. This tool, together with the range of support materials from Start4Life, can provide breastfeeding advice at any time of night or day and support mothers and their partners and families through challenges they may face.
We do hope you will join us during the week and help to celebrate breast feeding! Please read the blogs, tweet via social media using #CelebrateBreastfeeding, share our resources and create a social movement to embrace breastfeeding!
Viv Bennett is Chief Nurse/Director for Maternity and Early Years at Public Health England
2 comments
Comment by Lizzie Perdeaux posted on
We need to improve communication around infant feeding and stop creating an ‘Us and Them’ culture between mums who breastfeed and those who formula feed. I understand that ‘Breast is Best’ and I desperately wanted to breastfeed my son, but unfortunately I caught cellulitis in my left breast (as a result of nipple trauma caused by breastfeeding) that quickly became life threatening and killed off a large part of the skin on my breast (I still haven’t fully healed nearly 4 months on). I was in hospital and separated from my son for 2 weeks so he had to be formula fed during this time. When I got home, I was so scared about going back into hospital and being apart from him again that I decided to carry on formula feeding him rather than trying to feed him just on one breast.
I am a medical writer, so I have some understanding of stats and the difference between what happens in populations vs individuals. If I didn’t have this training (which most people don’t), it might seem to mums who are formula feeding their babies that their child is bound to grow up to be stupid and fat with constant ear infections, that they will get breast/ ovarian cancer, and that the Mum–Baby attachment will be insecure. Surely there must be a way of communicating about breastfeeding in a way that is also respectful to mums who are bottle feeding, and doesn’t have the subtext that mums who can’t/ don’t breastfeed are actively harming their children? In my experience and that of my peers, most mums bottle feed out of necessity rather than convenience (what’s convenient about making up a bottle at 3 am anyway!) and struggle with feelings of grief and guilt when they can’t breastfeed.
I agree and support the fact that breastfeeding rates should be improved, and we definitely need to create a society where breast feeding is easier, so I applaud your campaign and am looking forward to seeing what else you have planned for this week. However, I don’t think that simply banging the ‘Breast is Best’ drum repeatedly will affect breastfeeding rates that much. Mums need to know the realities of breastfeeding before they start (ie that it’s a skill to be learned and won’t just magically work first time for the majority of people). That way, if it is uncomfortable/ hurts, if it takes several weeks for milk supply to stabilise, or if they encounter complications, new mums will know what to do and have the confidence to persevere.
The communication about breastfeeding needs to have less emphasis on imparting information (breast is best, here’s the biology) and more on providing practical support (here’s how to do it) and reassurance (these things can go wrong, but here’s how you get through them - you're doing brilliantly, stick at it). Far from putting people off (most mothers would walk through fire for their children), I think it would give them a more accurate picture about the realities of breastfeeding. Then when it doesn’t work straightaway, they would be more likely to ask for help and persevere rather than thinking “breastfeeding doesn’t work, I am a failure” and give up.
The final message that’s missing from all info on infant feeding (and hopefully this will change with the Royal College of Midwives new policy) is “if you’ve tried your hardest and breastfeeding really isn’t working, or if breastfeeding just isn’t an option, formula is fine. True, it doesn’t have some of the health benefits that breastmilk has, but it’s better to feed your child than not!”
Breastfeeding rates will only improve when information on infant feeding becomes more compassionate, less paternalistic and aligned to what new mums are experiencing ‘on the front lines’.
Comment by Viv Bennett posted on
Thank you for your views and I agree with your comments and the need for sensitive stronger communication in all forms that help mothers with all aspects of this precious experience. The evidence is clear that breastfeeding is the best and complete nutrition for babies until around 6 months and it supports the immune system, with clear benefits. PHE recognises that mothers and babies form a unit, and baby’s wellbeing depends on the wellbeing of the mother. PHE is sharing the evidence and best practice examples so that commissioners of local services are able develop support systems for mothers, whenever they encounter difficulties in those special early weeks and months.