 We are increasingly aware that, across England, the proportion of children with excess weight is a major public health issue. Our concerns are based on a number of factors, which affect children now and later as adults.
We are increasingly aware that, across England, the proportion of children with excess weight is a major public health issue. Our concerns are based on a number of factors, which affect children now and later as adults.
Through the National Child Measurement Programme[i], overseen by PHE, we know that:
- One in five children in reception year (ages 4/5) is either overweight or obese
- By the time they reach the end of primary school, in year 6, this rises to 1 in 3
- Obesity rates double between reception and year 6
- Obesity rates are higher for boys than girls
- There are significant differences by ethnicity, which we need to gain a better understanding of
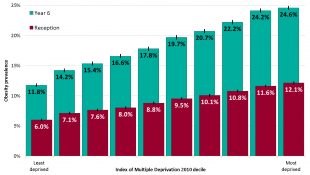
- Children from the poorest areas have a rate of obesity twice that of children from the most affluent areas, as the chart below shows
A longitudinal study[i] in South Gloucestershire of NCMP data shows how important it is that children arrive at reception year with a healthy weight. The study found that fewer than 16% of children who were obese in reception year had managed to reach a healthy weight by the end of primary school. Studies like these simply reinforce why PHE, and local authorities, are right to have a strong focus on giving every child the best start in life – and that includes a healthy weight.
PHE is working closely with local government, schools and parents, to see how we can provide more support and advice when parents receive information on their child’s weight status from the NCMP programme.
We also know that as children get older and go to secondary school, the combination of eating increasingly unhealthy foods and drinks, and less physical activity, leads to almost 19% of 11-15 year olds being obese[ii].
Research tells us that serious health and wellbeing problems are caused by excess weight in childhood – including asthma, musculoskeletal problems, psychosocial risks, sleep problems, CVD and of course greater risk of type 2 diabetes[iii]. Young people themselves describe the emotional problems, bullying and lack of confidence that obesity can lead to for some of them.
The scale of the issue is such that the Public Health Minister, Jane Ellison, told PHE’s recent annual conference (September 2015) that the government would be publishing a child obesity strategy later this year.
PHE is working closely with other government departments to support this. The factors behind child excess weight are complex and require a wide range of businesses, organisations and government departments to take action. Drawing on its expertise, knowledge and intelligence capabilities, public health is well placed to play a major role to help every child and young people have a healthy weight.
Watch this space for developments.
Eustace De Sousa, National Lead, Children, Young People and Families, Public Health England
[i] http://info.uwe.ac.uk/news/uwenews/news.aspx?id=3095
[ii] http://www.noo.org.uk/securefiles/150915_1154//ChildWeight_Aug2014_v2.pdf
[iii] https://www.noo.org.uk/NOO_about_obesity/obesity_and_health/health_risk_child

6 comments
Comment by Caron Torbohm posted on
Northumberland School Health service currently have a few nurses who have been trained as Healthy Weight champions and will be preparing to disseminate training to colleagues to support children, young people and their families and carers with making the right decisions.
Comment by Claire French posted on
As a school nurse, we find that some parents still comment that BMI is not an accurate way to record a child's weight and muscle mass and body type is not taken into consideration. How can we get parents on board with understanding the long term implications for being overweight in reception may equate to then being overweight in year 6 and then beyond?
Comment by Sarah Gill posted on
We need to teach parents how to cook healthy meals and then children will learn from their parents. But also supermarkets need to help by reducing the amount of unhealthy ready meals they sell
Comment by Lynn Wilkinson posted on
I find this topic very interesting and having worked in school nursing for the past 12 years I am able to see the issues in practice. I have helped developed the services we offer around children following the NCMP. I would love to be able to get that support in during the antenatal period and in the years before they start school to embed healthy lifestyles early. This proactive effort if done correctly could have more of an impact on society and what is seen as "normal", and not just individuals. The only concern I see in practice is the proactive work and support work for families which obese children, these are the services which have seen funding cuts. I fear that we collect the NCMP data, but what do we do with it. We know there is a crisis but are not effective in turning round the trends. Very interesting blog, thank you.
Comment by Sandra Williamson posted on
Interesting reading, Thank you. This was 18 months ago and we are still finding it difficult to support families in helping them and place all the responsibility on parents and schools and expect them to access websites - difficult for the poorest communities and those families who are overwhelmed with today's pressures.
Comment by Viv Bennett posted on
Sandra - Thank for you your response. As you point out we continue to see high levels of child obesity, with a significant social gradient. The Government's Child Obesity Plan (https://www.gov.uk/government/publications/childhood-obesity-a-plan-for-action) sets out a whole series of actions, including support for children and families, that should see positive changes to this situation but it will take action from all parts of society before we see major changes in these trends - Eustace